Jan 29, 2015Ahead of the Game
Assessing an athlete for a concussion is as much an art as a science. New tools hold promise for tipping the scales more toward science.
By Dr. Tamara Valovich McLeod, Michelle Weber, and Melissa Kay
Tamara Valovich McLeod, PhD, ATC, FNATA, is the Director of the Athletic Training Program and a Professor at A.T. Still University’s Arizona School of Health Sciences. She was a contributing author for the NATA Position Statement on the Management of Sport-Related Concussion and has done extensive research on head injuries. Michelle Weber and Melissa Kay are graduate students in the Post-Professional Athletic Training Program at A.T. Still. Dr. McLeod can be reached at: [email protected].
Your quarterback was sacked by a huge defensive lineman and lays unconscious. Standing on the sideline, you saw his head rotate as the opposing player made contact and you could instinctively feel how hard he hit the ground. It’s pretty clear he’s suffered a concussion.
You get a call from the women’s soccer field. A player twisted her ankle while landing after a battle for a header. The assistant coach relays that there was a fairly rough collision while the players were in the air, and now the athlete seems a little “off.” Mostly, she is upset over injuring her ankle. But could she also have sustained a head injury?
Some concussions are clear cut. Some are not. Yet athletic trainers have to do their best to assess the injury in a timely manner. Coaches want to quickly know: Has my athlete suffered a concussion? How bad is it? When can they return to play?
Of course, the answers to those questions are not always straightforward. Diagnosing a concussion entails knowing the mechanism of injury, understanding signs and symptoms, and conducting several clinical tests. There is no one quick exam that will tell all.
The good news is that there are many options emerging to help evaluate concussions. From better sideline tests to applications that combine tools, the field is bursting with new solutions. While many of the ideas still require more research to prove their effectiveness, they show promise in assisting athletic trainers and physicians to more quickly and accurately assess suspected head injuries.
BEST PRACTICES
Currently, there is consensus across several guideline and position statements that the best method of concussion assessment is multifactorial. Assessments should include the use of symptom inventories, cognitive tests, and postural control or balance assess- ments, along with a thorough clinical examination.
Symptom inventories can include checklists or scales, in which the athlete rates the severity and duration of each symptom. Best practices recommend asking questions about symptoms in an interview format, which helps mitigate underreporting of symptoms.
Cognitive tests run the gamut from simple to sophisticated. They include brief sideline assessments, such as the Standardized Assessment of Concussion (SAC), and more thorough pencil- and-paper tests such as Symbol Digit and Trail Making Test. Aspects of the SAC have been included in the Sport Concussion Assessment Tool, versions 2 and 3 (SCAT2 and SCAT3).
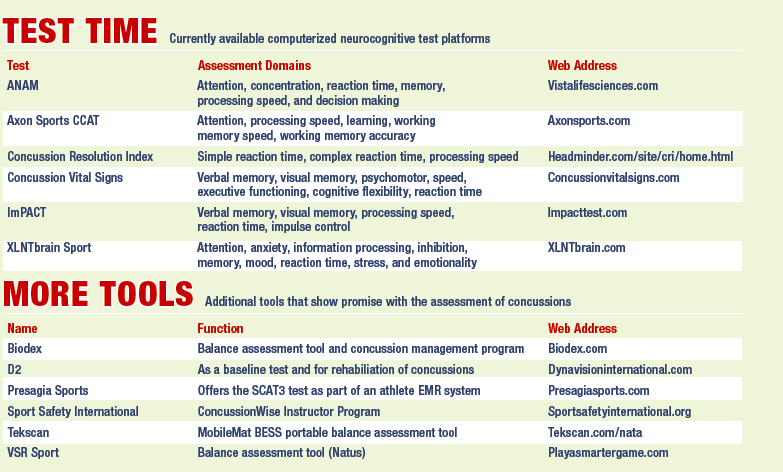
Computerized neurocognitive tests are commonplace in sports medicine today, with their use mandated by some professional sports leagues and widespread in both collegiate and interscholastic athletics. The role of neurocognitive tests has changed over the years from being seen as the go-to solution for concussion evaluation to one of many tools to use. But they are still an important element of assessment and play a large part in addressing the academic issues student-athletes can face after a concussion. (See “Test Time” for a summary of computerized neurocognitive tests.)
Although used less frequently, assessment of postural control or balance should be considered. These tests are easy to administer but have low-to- moderate diagnostic accuracy. However, they can be useful to gain a sense of impairments following concussion.
While these tools can certainly assist in the assessment process, there is insufficient evidence to suggest any one of them can be used alone to diagnose concussions. As a result, many new tests and technologies are emerging. They aim to improve the accuracy of concussion assessment and many are making their way into both mainstream practice and the scientific literature.
THE EYES HAVE IT
The assessment of oculomotor function, responsible for eyeball and eyelid movement, is an important part of a thorough clinical exam after a suspected concussion, and new tools provide objective data on it. The King-Devick Test involves quickly reading a string of numbers on three test cards to measure for saccades, attention, concentration, speech, and language. Its manufacturer promotes it as being easily administered by parents and coaches. However, healthcare professionals must be cautious in allowing assessment of a suspected concussion by non-medical personnel.
Several studies have been published on this test that have demonstrated excellent test-retest reliability and acceptable internal consistency. Concussed athletes have been found to record significantly slower times, indicating worse performance, compared to a preseason baseline. The current evidence, low cost, and ease of administration suggest the King-Devick Test is a promising tool to use as part of a battery of tests on the sidelines.
Oculomotor assessment may also be evaluated using computerized systems that include infrared goggles, rotary chairs, and other optokinetic devices. These more expensive systems are intended for use by audiologists, neurologists, and neuro-opthamologists, but may have promise in assessing concussed athletes. One recently presented abstract evaluated the iPortal Neuro- Otologic Test Center and found concussed patients had significantly lower scores, by two standard deviations, on at least three of the oculomotor or pupillary reflex tests compared to their baselines. These types of assessments may be of value for athletic trainers in a collaborative approach to concussion management with other healthcare providers who have access to advanced technologies.
IN ONE PACKAGE
Other emerging technologies incorporate the recommended multifaceted approach to concussion assessment into one system. Many of these products are just reaching the market and have yet to be tested in published studies. Yet they hold the potential to help athletic trainers by combining an array of tools into one package.
The C3 Logix System evaluates postural stability, working memory, set switching, reaction time, learning, and static and dynamic visual acuity within one program. The system uses an iPad app to analyze data from a variety of tests and presents it in an easy-to-read format. The analysis covers the graded symptom scale, balance test, simple reaction time, choice reaction time, Trail Making Test, and memory and processing speed.
CogniSens Athletics Inc., has several technologies aimed at assessing neural status and assisting in rehabilitation simulation of a concussed athlete. The NeuroMinder C3 system is a combination of three complementary technologies: NeuroMinder, which evaluates neural activity through visual imagery testing; NeuroBalance, which assesses postural control using visual stimuli; and NeuroTracker, which trains perceptual skills and may be useful in concussion rehabilitation.
The XLNTbrain system is a comprehensive tool kit that includes elements for recognizing, reporting, and recovering from a concussion. Delivered online or through a mobile application, it features concussion education through video training, as well as balance assessment, neurocognitive testing, and emotional indicators. A sideline assessment mobile app allows post-injury evaluation of symptoms and balance, along with a web-based post-injury neurocognitive test. During the recovery process, symptoms can be monitored daily and the system will generate a plan for limiting academic work based on the type, number, and severity of reported symptoms.
The X2 Integrated Concussion Examination (ICE) is a cloud-based concussion management system that includes the SCAT2, SCAT3, and the NFL concussion assessment protocol. It allows for the examination of symptoms, cognitive performance, short-term and delayed recall memory, balance and coordination, and situational orientation. It is compatible with mobile devices and can be used to compare post-injury scores with baseline assessment scores.
IMPACT INDICATORS
Several brands of head impact indicators are available that sense force and acceleration resulting from impacts to the head. These devices are not meant to diagnose concussion, but rather to alert a medical professional that an athlete should be examined for signs of a concussion, as well as to detect the frequency and magnitude of impacts to the head.
It is important to note that there is little evidence to suggest a reliable impact threshold for a concussion exists. Each concussion is different–some may result from higher magnitude impacts, while others may occur at lower force levels.
However, some studies now suggest that concussions are more likely to occur with impacts between 70 to 100g. To date, the only published studies evaluating head impact sensors have been done with the Head Impact Telemetry (HIT) System, which has been used solely as a research tool. (See “The Impact” for a look at many of these devices and the sports in which they can detect impacts.)
ON THE HORIZON
There are several larger trends that will influence the assessment of concussions going forward. One is the increased use of smart phones and tablets. The other is the proliferation of electronic medical records (EMR) systems.
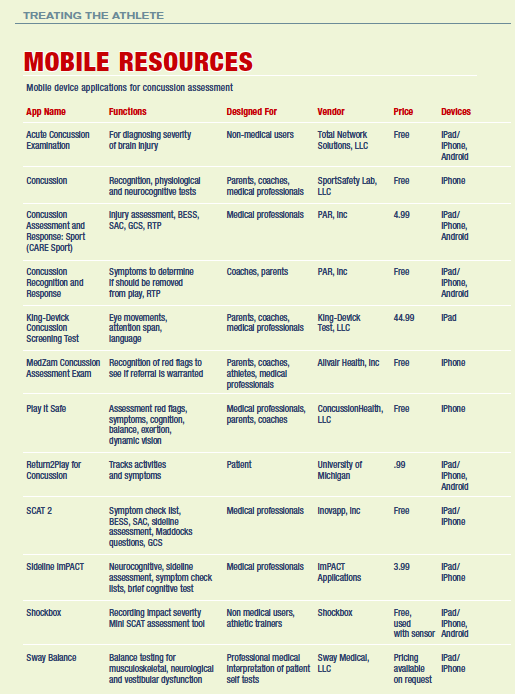
Several of the neurocognitive test platforms have a mobile app specifically for the sideline assessment that is designed to accompany the computerized test. Other apps are stand-alone products that either assess one component of the concussion evaluation (such as balance) or have a variety of tests. (See “Mobile Resources” for a summary of the function and intended user for many of these mobile apps.) There is little published evidence supporting specific apps, but many are based on assessments such as the SAC or SCAT2, which have been found to identify deficits in concussed athletes compared to a baseline score.
And finally, several EMR systems have now added concussion-specific components to allow for easy administration and reporting of symptoms, such as cognition or balance. For example, Presagia Sports includes the SCAT3, and the Athletic Trainer System (ATS) incorporates the SCAT2, BESS, and SAC, as well as Maddocks’s questions and an exertional protocol. CORE-AT EMR has forms that are based on the concussion documentation recommendations from the NATA position statement on managing sport- related concussion, and it also utilizes the SCAT2.
All of these new tools will likely change the way concussions are assessed and managed in the future. For now, athletic trainers can consider incorporating some of these assessments into their protocols. And, with more research, many of them may prove reliable in the not-too-distant future.
For a list of references for this article, please visit: www.Training-Conditioning.com/ references.